gut health
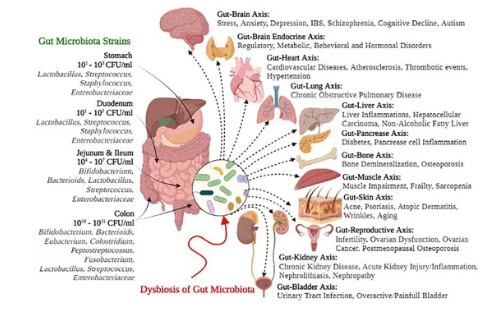
Centuries ago, Hippocrates famously said, “All disease begins in the gut,” and modern medicine is now catching up with the profound truth behind that statement. The gut, often referred to as the “second brain,” is home to trillions of microorganisms collectively known as the gut microbiota. These microbes are essential for digestion, nutrient absorption, immune regulation, and even neurotransmitter synthesis. When the balance of these microorganisms is disrupted—a condition known as dysbiosis—it can lead to a wide range of health issues, including neurological disorders.
While medical professionals may differ in their approach to treating chronic illnesses or autoimmune conditions, many agree that healing the gut is a foundational step in healing. The exception may be cases involving mold toxicity, where addressing the mold takes precedence.
The Gut-Brain Connection
The intricate relationship between the gut and the brain is facilitated by the gut-brain axis, a complex biochemical network involving the nervous, endocrine, and immune systems. Communication along this axis is bi-directional: the brain influences gut function, and the gut sends signals back to the brain. These messages are transmitted through neural pathways, hormones, and immune mediators, allowing the gut microbiota to have a profound impact on brain health and emotional well-being.
Gut Microbiome
The gut is a dynamic ecosystem teeming with bacteria, viruses, fungi, and other microorganisms. Each of these plays a unique role in maintaining health. Beneficial bacteria, known as probiotics, help with digestion, while other microbes can cause harm if their numbers grow unchecked. Achieving and maintaining balance in the gut microbiome is critical for overall well-being.
Gut Microbiome and Immunity
The gut is the body’s largest immune organ, home to a vast population of immune cells that help regulate immune function. The gut microbiota plays a key role in maintaining immune balance, known as immune homeostasis. Through complex interactions, gut bacteria help train immune cells, regulate inflammation, and promote tolerance to harmless substances.
When this delicate balance is disrupted, it can lead to immune dysregulation and contribute to autoimmune diseases such as inflammatory bowel disease (IBD), rheumatoid arthritis, and type 1 diabetes.
Neurotransmitter Production and Function
A healthy gut microbiome is essential for the synthesis and regulation of neurotransmitters like serotonin and dopamine, which are crucial for mood and cognitive functions. Serotonin, often called the “happiness neurotransmitter,” is mostly produced in the gastrointestinal tract, with gut bacteria playing a key role in converting dietary tryptophan into serotonin precursors. Similarly, dopamine, the “reward neurotransmitter,” is produced in both the brain and the gut. Gut microbes also influence other important neurotransmitters like GABA and acetylcholine, highlighting the vital role of the gut in mental health.
Common Gut-Related Problems
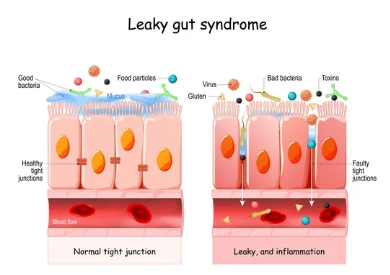
Leaky Gut
The intestinal barrier is a selective gatekeeper, allowing nutrients to enter the bloodstream while blocking harmful substances. When this barrier is compromised—a condition known as leaky gut—bacteria, toxins, and undigested food particles can pass through the intestinal lining, triggering inflammation and contributing to systemic health issues. Studies, including those from Harvard Health, suggest that leaky gut is on the rise, largely driven by the Standard American Diet (SAD), which is high in sugar and saturated fat and low in fiber.
In some individuals, gluten can trigger the release of zonulin, a protein that loosens the tight junctions between gut cells, exacerbating leaky gut. This condition has also been linked to autoimmune diseases.
Nutrient Absorption
The gut is responsible for absorbing essential vitamins, minerals, and nutrients, which fuel every cell and support bodily functions. Specialized cells in the small intestine, called villi and microvilli, help maximize nutrient absorption. However, when gut health is compromised, malabsorption can occur, leading to nutrient deficiencies that impair immune function, cellular health, and overall well-being.
Key nutrients like vitamin D, zinc, omega-3 fatty acids, and amino acids such as glutamine are essential for gut health. Deficiencies in these nutrients can weaken the gut lining and contribute to chronic conditions.
Psychological Stress and the Gut
Stress, whether acute or chronic, can significantly impact gut function via the gut-brain axis. Stress hormones like cortisol can weaken the intestinal barrier, increase gut permeability, and disrupt the balance of gut bacteria. This can lead to digestive issues and exacerbate conditions like leaky gut and dysbiosis.
Chronic Infections and the Gut
Chronic infections, such as those caused by H. pylori, E. coli, or Candida albicans, can inflame the gut, disrupt the microbiome, and weaken the gut lining. These infections trigger ongoing immune responses, which can contribute to autoimmune diseases. Managing chronic infections is essential for restoring gut health and alleviating symptoms of autoimmune conditions.
Role of Histamine in Gut Inflammation
In the gut, histamine is released by mast cells and plays a normal role in physiological processes. However, when histamine levels become unbalanced, it can increase intestinal permeability and promote inflammation. Managing histamine levels through diet and supplements like DAO enzymes can help reduce gut inflammation and alleviate symptoms associated with autoimmune diseases.
Environmental Stressors on the Gut
Environmental factors can also impact gut health. Processed foods, chemical exposures (such as pesticides or NSAIDs), and pollutants like heavy metals can damage the gut lining and disrupt the microbiome. Even lifestyle factors like poor sleep and chronic physical exhaustion can negatively affect gut health by altering immune function and microbial balance.
Practical Considerations
Constipation
Constipation isn’t just an inconvenience—it has serious implications for gut health. When waste stagnates in the colon, toxins are reabsorbed into the bloodstream, contributing to systemic toxicity and inflammation. Regular bowel movements (1–2 times daily) are critical for expelling toxins and maintaining overall health.
Gas and Bloating
When waste lingers in the colon, fermentation by gut bacteria produces gases that lead to bloating and discomfort. This environment can also promote dysbiosis, creating an imbalance between beneficial and harmful gut bacteria. Addressing these issues helps restore gut balance and relieve symptoms.
Conclusion: The Path to Gut Health
Gut health is foundational to overall well-being, impacting everything from immunity and mental health to nutrient absorption and chronic disease prevention. Healing the gut begins with nurturing the delicate balance of the gut microbiome, repairing the intestinal lining, and addressing stressors like diet, infections, and environmental exposures.
By taking a holistic approach that prioritizes gut healing, we can support not only digestive health but also the intricate systems throughout the body that depend on a healthy, balanced gut. Healing truly begins in the gut, and by caring for it, we lay the foundation for lasting health and vitality.
