inflammation
Acute Inflammation
Acute inflammation is the body’s immediate and localized response to an injury or infection. When the immune system detects a threat such as a wound, bacteria, or virus it responds by sending immune cells to the affected area. These immune cells release signaling molecules like cytokines, which promote swelling, redness, and heat. This inflammatory process is necessary for repairing tissues, eliminating pathogens, and protecting the body from further damage. Once the threat is neutralized, the immune system typically returns to a state of balance, and the inflammation subsides.
However, while short-term inflammation is protective, prolonged or chronic inflammation is very harmful for the body and has significant downstream effects.
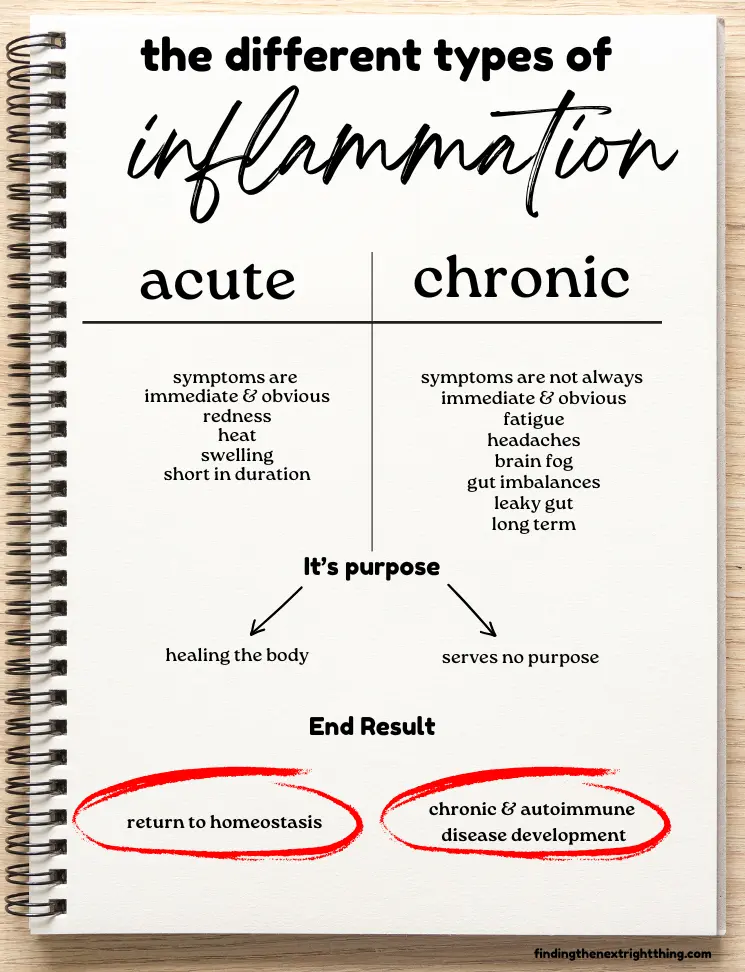
Chronic Low-Level Inflammation: The Silent Disruptor
In contrast to acute inflammation, low-level chronic inflammation sometimes called “silent” inflammation operates at a more subtle level. This type of inflammation does not produce obvious symptoms like pain or swelling, yet it can persist in the body over long periods.
Unlike the inflammatory response to an acute trigger, chronic inflammation is associated with mold, gut imbalances, environmental toxins, chronic stress and some low-grade persistent infections like Lyme, Epstein Barr, or CMV. Over time, this low-level inflammation can create a pro-inflammatory state in the body, where immune responses are continuously activated but without the clear signs of acute inflammation.
One of the dangers of chronic inflammation is that it can go unnoticed, leading to gradual damage in tissues and organs. This prolonged immune activity also creates a fertile ground for the development of autoimmune diseases, where the immune system begins to attack the body’s own tissues organs.
Autoimmunity and the Role of Chronic Inflammation
Autoimmune diseases occur when the immune system’s ability to distinguish between “self” and “non-self” breaks down; the immune system misidentifies healthy cells as threats and launches an attack. Chronic, low-level inflammation is a key factor in this process. When the immune system remains in a heightened state of activation over time, the risk of developing autoimmunity increases, as immune cells can become confused and start targeting the body itself.
For example, research has shown that elevated levels of inflammatory markers such as tumor necrosis factor-alpha (TNF-α) and interleukin-6 (IL-6) are often present in both chronic inflammation and autoimmune conditions. These pro-inflammatory molecules can further perpetuate inflammation, creating a cycle of immune system overactivity that is difficult to break.
In modern society, we are constantly exposed to factors that promote low-level chronic inflammation. Many elements of our daily lives, from the food we eat to the air we breathe, contribute to this state of constant immune activation. Some of the primary causes include:
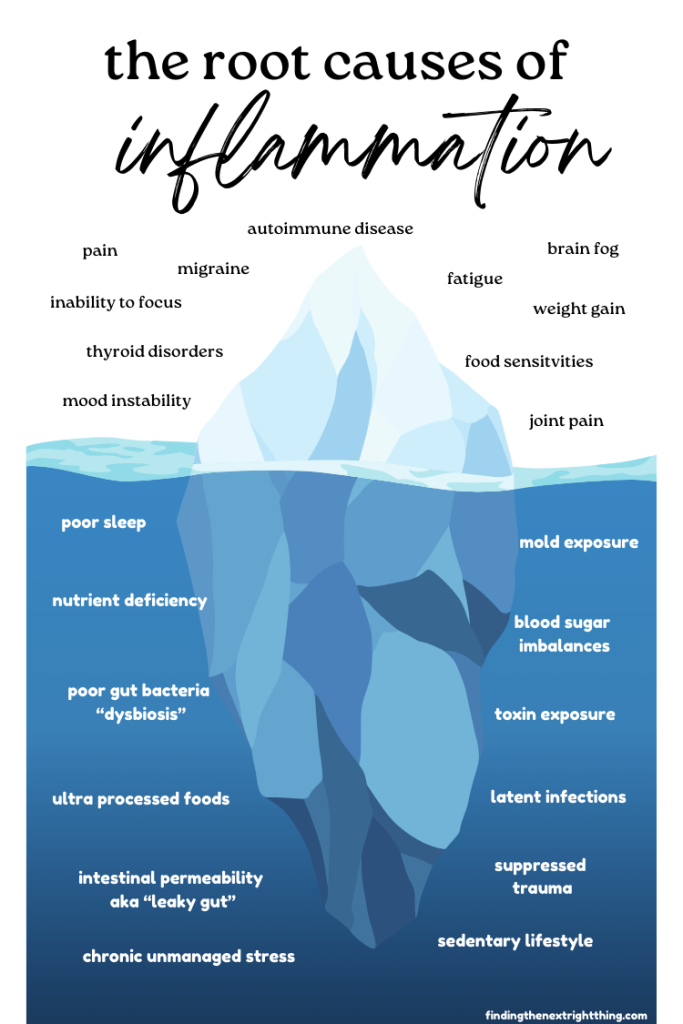
- Dietary Factors: Diets high in sugar, refined starches, genetically modified foods, and processed foods are known to trigger inflammation. These foods can promote insulin resistance and metabolic imbalances, which are closely linked to inflammation. For example, the consumption of sugar and high-glycemic foods causes spikes in blood sugar, leading to the release of pro-inflammatory cytokines such as TNF-α. Additionally, endotoxins like lipopolysaccharides (LPS) can be absorbed through a leaky gut and trigger systemic inflammation.
- Sedentary Lifestyle: Lack of physical activity further exacerbates inflammation. Exercise helps regulate insulin sensitivity, reduce oxidative stress, and promote a healthy inflammatory response. A sedentary lifestyle, on the other hand, increases the risk of chronic low-level inflammation, contributing to metabolic conditions like obesity and type 2 diabetes.
- Environmental Toxins: Pesticides, heavy metals, and pollutants from household products also contribute to chronic inflammation. Toxins can accumulate in tissues, disrupting normal cellular function and triggering immune responses. For example, exposure to heavy metals like mercury and lead can cause oxidative stress, which in turn promotes inflammation.
- Stress: Chronic stress releases cortisol, a hormone that, in short bursts, helps control inflammation. However, when cortisol levels remain elevated due to prolonged stress, the immune system becomes dysregulated, leading to increased inflammatory responses. Psychological stress is often linked to elevated levels of inflammatory markers, such as C-reactive protein (CRP).
- Latent Infections: Many people harbor latent infections—such as Epstein-Barr virus (EBV) or herpes simplex virus (HSV)—without being aware of it. These infections can periodically re-activate, prompting the immune system to respond and contributing to chronic inflammation.
- Microbiome Imbalances: Imbalances in the gut microbiome, such as dysbiosis or leaky gut syndrome, allow harmful endotoxins like LPS to enter the bloodstream. Once in the bloodstream, these endotoxins activate immune responses that promote inflammation and further disturb the immune system’s balance.
- Mold Exposure: Exposure to mold and mycotoxins can lead to an inflammatory response as the body tries to eliminate the harmful substances. Mycotoxins have been shown to affect the immune system directly, promoting an inflammatory state that can contribute to immune dysregulation and exacerbate chronic illness.
Low-Level Inflammation and Autoimmune Disease: A Vicious Cycle
Neuroinflammation and Mental Health
In recent years, research has increasingly shown that inflammation is not just a factor in physical ailments like autoimmune diseases and chronic illnesses, but it also plays a significant role in conditions like depression and anxiety. Traditionally, these mental health conditions were thought to be solely the result of chemical imbalances in the brain. However, a growing body of evidence suggests that inflammation may be a key contributor to the development and persistence of these disorders.
Studies have found that individuals with depression and anxiety often have elevated levels of inflammatory markers, such as cytokines and C-reactive protein (CRP). These inflammatory molecules appear to cross the blood-brain barrier and affect brain function, particularly in areas that regulate mood and behavior.
Inflammation and PANS/PANDAS
For children with PANDAS, inflammation, particularly neuroinflammation, can lead to a range of challenging neurological symptoms such as obsessive-compulsive behaviors, tics, anxiety, and mood swings. This inflammation occurs when the immune system, after a strep infection, mistakenly targets parts of the brain, confusing them for harmful invaders.

PANS, while similar to PANDAS, can be triggered by a broader range of factors, including infections and environmental influences. Each of these can spark a sudden onset of neuropsychiatric symptoms for a PANS child.
In both PANDAS and PANS, reducing this inflammation is the priority. It’s not just about alleviating symptoms; it’s about allowing the body to redirect its energy toward healing, rather than using its resources to deal with an overactive immune system.
Brain inflammation in PANS/PANDAS involves several complex immune mechanisms:

- Autoantibody Production: The immune system mistakenly produces antibodies that target the brain tissues, particularly the basal ganglia, a region essential for regulating movement and behavior. This misdirected attack can lead to the neurological symptoms seen in PANS/PANDAS.
- Cytokine Release: In response to infection or injury, the body’s immune cells, particularly microglia, release cytokines—proteins that help cells communicate and coordinate an immune response. However, when cytokine production becomes dysregulated, it can result in prolonged inflammation. Excess levels of certain pro-inflammatory cytokines in the brain can exacerbate the inflammation and symptoms associated with PANS/PANDAS.
- Blood Brain Barrier Disruption: Inflammation can compromise the integrity of the blood-brain barrier (BBB), which normally acts as a protective shield, preventing harmful substances from entering the brain. When the BBB is disrupted, it becomes easier for pathogens and immune cells to penetrate the brain, leading to further inflammation and neurological challenges.
PANDA Flares
When a child is in a flare, the priority is to lower that inflammation as quickly as possible. Lowering the inflammation not only reduces the severity of the symptoms, but it also allows the body to conserve its energy for healing, instead of burning through ATP when the immune system is in overdrive.
Kids with PANS/PANDAS deal with both acute and chronic inflammation. Outside of the flares, even if a child is not exhibiting the full intensity of symptoms, low level chronic inflammation may persist contributing to ongoing but subtler symptoms. This chronic inflammation can be due to immune dysregulation, lingering infections, or unresolved underlying triggers, and it can make the child more vulnerable to future flares. True remission typically occurs when both the acute and chronic inflammation are fully resolved, allowing the immune system to return to balance.
Put out the Flame

- Reduce stressors—food, stress, toxins, heal the gut
- Put out the flame with anti-inflammatory herbs
The anti-inflammatory herbs in the Herbal Guide can be a part of this approach. Whether it’s calming an acute flare or managing long-term inflammation, these natural remedies can support the body in its healing process, helping to reduce the overall inflammatory burden.
PANS, while similar to PANDAS, can be triggered by a broader range of factors, including infections and environmental influences. Each of these can spark a sudden onset of neuropsychiatric symptoms for a PANS child.
In both PANDAS and PANS, reducing this inflammation is the priority. It’s not just about alleviating symptoms; it’s about allowing the body to redirect its energy toward healing, rather than using its resources to deal with an overactive immune system.
